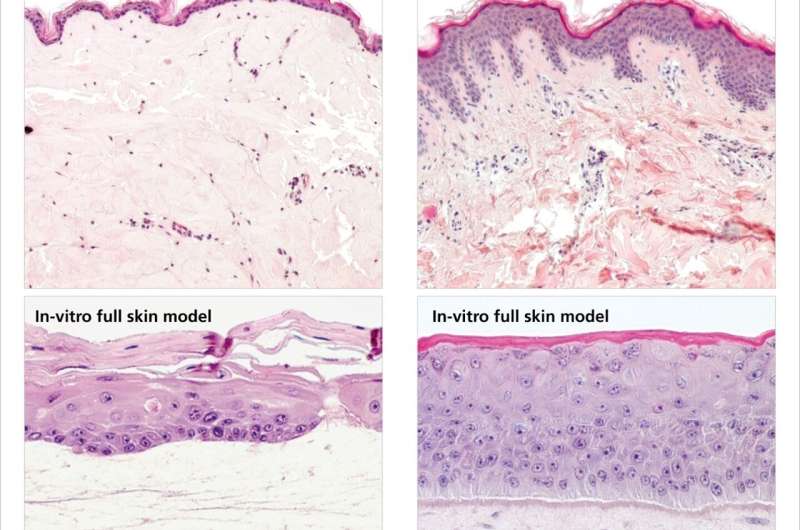
Histological sections of native canine skin (top left) and human skin (top right) show that dogs have a thinner epidermis with hardly any protective function. Microscope images of in-vitro cultivated skin equivalents (bottom) show that lab-grown canine skin (bottom left) is morphologically almost identical to the original. Credit: Fraunhofer IGB
Reproducible in-vitro canine skin has been grown in a laboratory setting for the first time by researchers at the Fraunhofer Institute for Interfacial Engineering and Biotechnology IGB.
The research team developed a full-thickness dog skin equivalent based on native skin cells. This makes it possible to precisely test medical treatments in vitro on the sensitive skin of dogs. The skin equivalent can even be used to test the compatibility of care products such as shampoo or soap—eliminating the need for animal testing.
Whether they're out in the wind and rain or rolling around in the grass, on the outside dogs seem to be resilient creatures. But underneath it all, our four-legged friends have an above average tendency to suffer from skin conditions.
About 10% to 15% suffer from atopic dermatitis, a form of neurodermatitis in which the skin becomes dry and scaly, causing the dog to scratch. The condition is often accompanied by inflammation. Although creams and ointments are available to treat the condition, their success rate is uncertain—in fact, some treatments have no effect at all and in the worst cases can make symptoms worse.
This is exactly what Dr. Anke Burger-Kentischer, head of the Cell and Tissue Technologies department at the Fraunhofer Institute for Interfacial Engineering and Biotechnology IGB, and her team set out to do. In the WowWowSkin project, they succeeded in developing in-vitro dog skin in a laboratory setting for the first time, laying the foundations for using in-vitro models to develop and test medical treatments and care products for dogs.
"We wanted to create a reproducible canine skin equivalent that would be suitable for specific testing of therapeutic products for dogs. Nothing like this existed before," explains Dr. Burger-Kentischer.
The lab-grown full-thickness skin equivalent is almost identical to real dog skin, allowing accurate and meaningful testing of active ingredients in medicines. It is also suitable for testing the compatibility of commonly used grooming products, such as shampoos or soaps. These too can potentially damage a dog's skin if their effects are unknown, as the top layer of skin—the epidermis—is much thinner in dogs than it is in humans and has only little protective function.
Cultivating skin cells
The research team carried out the first stage of the project using a piece of native dog skin. The essential components in creating a full-thickness skin equivalent are the two upper layers of the skin: The protective layer called the epidermis, which contains keratinocytes that form the skin's horny layer, and the underlying dermis, which is filled with connective tissue, including cells called fibroblasts.
"After mechanically separating the layers, we used special enzymes to detach the cells from the surrounding tissue. We then immortalized them and multiplied them in culture dishes using a specific culture medium. This process created immortal keratinocytes from the epidermis and immortal fibroblasts from the dermis, which we joined together to create a full-thickness skin equivalent," Dr. Burger-Kentischer explains."We had to do a lot of testing to find the right combination of enzymes and media."
Despite the challenges, the results in the lab were a complete success, producing a full-thickness skin equivalent that was virtually indistinguishable from real dog skin under a microscope.
The Fraunhofer researchers are now able to colonize the full-thickness skin equivalent with pathogens and create a disease model that they can use to test medical treatments for conditions such as dermatitis.
"We can mimic inflammatory processes on skin equivalents by contaminating them with bacteria. When we then apply drugs or active substances to them, we can quickly see whether the treatment has an effect and reduces the number of bacteria, whether it has no effect at all—or whether it even makes the disease worse," says Dr. Burger-Kentischer.
The original skin samples were provided by vets who had cut off pieces of skin during medically necessary surgery, for example. In other words, the only tissue involved was skin that had to be surgically removed anyway—nothing else was taken specifically for the project.
Provided by Fraunhofer-Gesellschaft